There are many advantages to being able to plan for a pregnancy before becoming pregnant. While not always possible, planning a pregnancy offers numerous benefits, including emotional readiness, financial preparation, and significant medical advantages. For the mother, ensuring proper nutrition, treatment, and vitamin intake, such as folic acid (Vitamin B9), is vital for healthy fetal development.
In the first month of pregnancy, an important process is going on; the neural tube, which develops into the brain and spinal cord, begins forming. When the development of this structure goes awry, the brain and spinal cord do not develop properly. Disruptions in this process can cause neural tube defects (NTDs) in which the baby’s spine does not close as it should and there is a gap in the spine. The most common outcome of this defect is that the baby will be born with a condition called spina bifida (split spine). Spina bifida occurs in about 1 in every 2,875 births. About 1,500 babies are born with spina bifida each year.
Before the symptoms and treatment of spina bifida are discussed, it is important to note that there is an easily obtainable way to increase the odds of your child not being born with spina bifida. Research shows that taking 400 micrograms of folic acid daily before and during early pregnancy can reduce the risk of spina bifida by up to 70%. Women with a history of spina bifida-affected pregnancies are advised to take 4,000 micrograms daily. While a healthy diet is extremely important, diet alone may not provide adequate folic acid; prenatal supplements are essential.
RISK FACTORS
Several factors increase the risk of spina bifida, including:
- Obesity: Women with a BMI of 30 or higher have an elevated risk.
- Diabetes: Poorly controlled blood sugar levels can increase risks.
- Family History: A close relative or having a prior child with spina bifida increases the risk of spina bifida.
- Medications: Certain drugs, such as valproate and carbamazepine (used for epilepsy and bipolar disorder), are linked to spina bifida. If there is a chance you could become pregnant while taking them, discuss alternative medication options and reliable contraception with your medical practitioner.
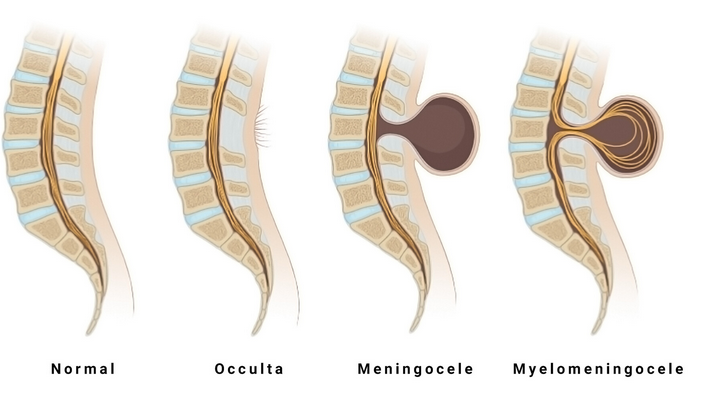
TYPES OF SPINA BIFIDA
- Occulta: The most common form of spina bifida. With a small spinal opening on the baby’s spine, occulta is often without symptoms.
- Meningocele: A sac of fluid protrudes through an opening in the spine; nerves are not typically affected, though reduction of bladder or bowel control may occur.
- Myelomeningocele: Nerves and spinal cord tissue in a sac protrude through an opening along the spine. Usually, the protrusion is in the lumbo-sacral region.